Will I Be Able to Golf Again After Reverse Shoulder Replacement
The major difference between a standard shoulder replacement and a reverse procedure is that in a reverse shoulder replacement the ball and socket parts of the shoulder joint switch sides. This means their natural position is reversed. Reverse total shoulder replacement is a complex procedure and is warranted by certain conditions. Call to request an engagement with one of our shoulder experts if you lot have shoulder problems that may require shoulder replacement.
Why are these shoulder replacements chosen a "reverse" prosthesis?
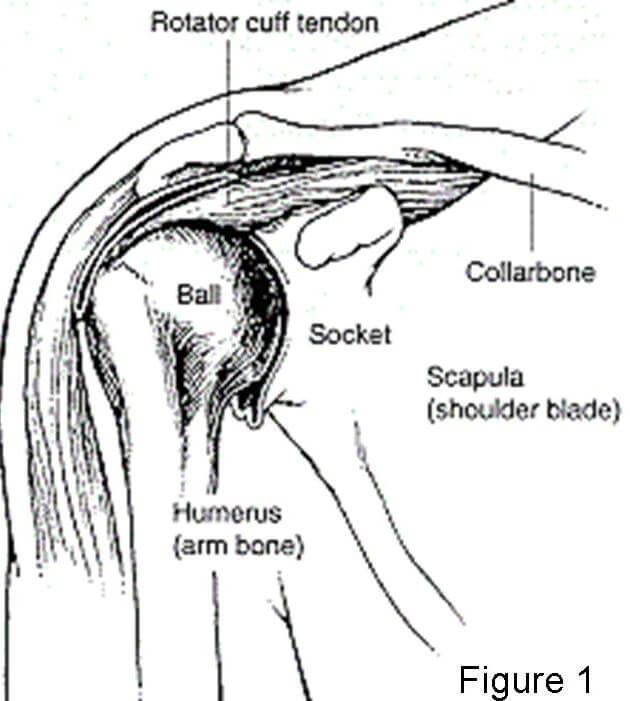
Shoulder replacements are designed to remove portions of the bones of the shoulder articulation that are arthritic (missing cartilage). The shoulder articulation is a ball and socket joint, with a ball (or humeral head) that is role of the humerus and a flat surface (which is chosen the socket) which is part of the shoulder bract (Figure 1). In a standard shoulder replacement, the ball portion of the shoulder (the humeral head) is replaced by a metal ball and the socket is replaced by a plastic piece (Figure ii).
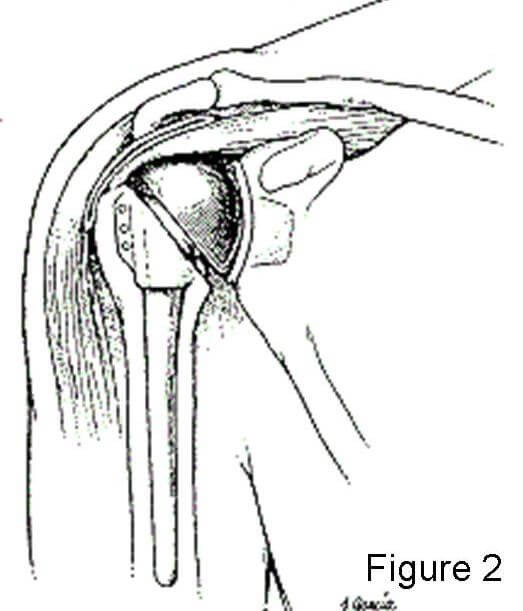
In the "reverse prosthesis" the shoulder joint is nevertheless replaced with parts or components made out of metallic and plastic (Figure 3). The big differences between a contrary prosthesis and a standard shoulder replacement is that in a reverse prosthesis, the ball is placed on the socket side of the articulation. This is opposite where it is located in nature, or "reverse" of what you would expect. The socket is and then placed on the arm side where it is supported by a metal stem in the arm bone (the humerus) (Figure 4). Thus the ball and socket are reversed from what occurs in nature.


How does it stay together?
Fortunately the reverse prosthesis tin can exist put into place with screws on the socket side which concord information technology into the bone of the shoulder blade (Figures 3 and 4). The ball then screws into the plate which has been fastened to the socket (Figure 3).
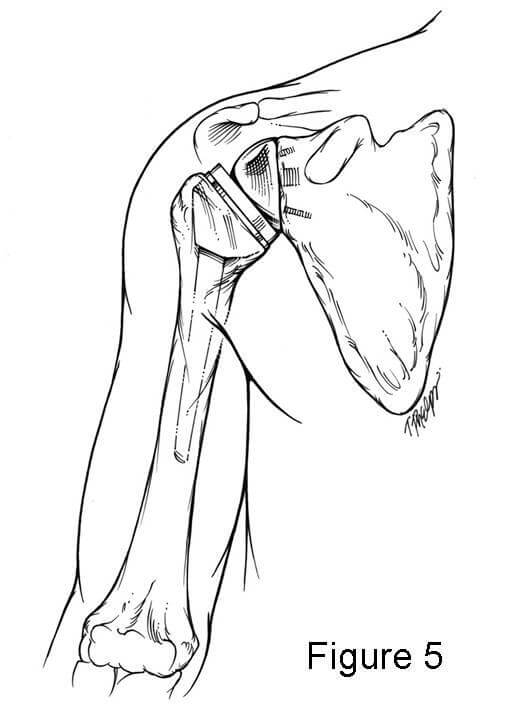
The part of the prosthesis placed into the arm bone is secured with cement which bonds the metal to the bone within a few minutes (Figure 4). The plastic socket piece then is press fit into the finish of the stem where it is securely fixed past locking into the metallic piece. This allows the socket to rotate on the brawl then that the shoulder motion tin exist restored (Figure 5). The muscles around the shoulder likewise help keep the reverse prosthesis in identify.
Why should a person get a reverse prosthesis instead of a standard shoulder replacement?
A standard full shoulder replacement depends upon muscles and tendons around the shoulder joint to be intact. The muscles attach to the shoulder blade and plough into tendons which attach to the shoulder. These muscles and their tendons part to move the shoulder and are together chosen the rotator cuff. When these tendons become extensively torn and then that they do not attach to the bone any longer, the shoulder frequently does not function normally. The loss of the rotator cuff can produce hurting and likewise loss of motion. A normal shoulder replacement is designed to work only if those tendons are intact. In contrast, a opposite prosthesis is designed for situations where the rotator cuff is torn or malfunctioning.
Play Video:
What shoulder atmospheric condition warrant contrary total shoulder replacement?
The main reason to consider a opposite prosthesis is when there is arthritis of the shoulder articulation and the rotator cuff tendons are torn or gone. This is the almost mutual surgical indication for a patient considering a contrary prosthesis. In this situation this functioning will requite the patient pregnant pain relief and may besides help with range of motion of the shoulder. While range of movement subsequently a reverse prosthesis may non be completely normal, it is typically improved over the move previously lost due to the arthritis and pain.
Another reason to have a reverse prosthesis is if the rotator cuff tendons are all torn and 1 cannot lift the arm high enough to function. Typically in this case the shoulder is not painful just the inability to lift the arm is very disrupting to the ability to role in life. When the patient goes to lift the arm at that place is a prominence on the front of the shoulder, and this is called an anterior-superior migration or subluxation of the shoulder. In these cases hurting may or may not exist a major factor for the reverse prosthesis, but the main reason for the replacement is to regain motion and function.
The 3rd most mutual reason to take a reverse prosthesis is if the shoulder has already had a replacement prior to the time a reverse prosthesis was available and the patient still has pain and loss of movement. Sometimes the regular shoulder replacement was placed for a fracture or for torn rotator cuff tendons and the shoulder continues to be painful. In this case, if a opposite prosthesis is needed, the surgery to place a reverse prosthesis is a little more complicated. The reason for this is that the kickoff, more traditional shoulder replacement has to be removed at the time of surgery, and the reverse can and so be placed in the shoulder.
Other reasons to have a reverse prosthesis are some fractures of the shoulder area, particularly ones that involve the proximal humerus (arm bone) where the ball attaches to the shaft of the os. In some instances, the bone is broken into many pieces or the ball may be separate into parts.
The last reason to accept a contrary prosthesis is considering of a tumor in the proximal humerus that involves the bone of the shaft of the bone or the ball of the humerus itself.
What is the surgery similar?
The surgery experience is very like to that of a regular shoulder replacement with a few variations. The primary factor in the recovery is whether this is the first shoulder replacement for the shoulder or whether an old prosthesis has to be taken out during surgery. When this is done, it is chosen a "revision" example and the recovery may be dissimilar than when a start time (called a "master") joint replacement is done.
The surgery is typically done with a nervus block of the arm followed by a general coldhearted. The incision is in the front of the shoulder and the surgery takes most two to three hours. Postoperative pain relief is obtained with pain medications orally and past vein if needed. Most patients tin begin moving the fingers, wrist and elbow the next 24-hour interval.
Whether shoulder motion begins the 24-hour interval after surgery depends upon how well the base of operations plate and ball are stock-still to the socket by the screws. In a contrary prosthesis there is some dependence upon the bone healing around the base plate and screws. As a result, movement of the shoulder may exist halted for a few days to a few weeks. Despite these precautions, most patients are allowed to use their extremity to swallow, read or apply a keyboard within a few days later on surgery. The amount the patient tin can lift the arm depends upon many factors and each patient is dissimilar. The corporeality of movement allowed by the patient after surgery also depends upon the fixation of the screws to the bone which tin can be determined at the time of surgery. Lastly, the amount of movement recovered after this surgery also depends upon how much motion the patient had prior to surgery.
Most patients donate a unit of claret prior to surgery which can be given back to them if needed. For first time joint replacements claret is given dorsum to the patient unremarkably only 10 to 20% of the time. For revision cases where the surgery is longer, nearly 80% of cases need a blood transfusion. Similarly, the length of fourth dimension for surgery is longer for revision cases (three to five hours) and the recovery fourth dimension for gaining function of the arm is longer. Other factors which influence the recovery time include whether os grafting (adding bone where it is missing) is done, whether it holds well and how long it takes the os to heal.
What results tin I expect from reverse total shoulder replacement?
The contrary prosthesis is very good at providing hurting relief. Studies from Europe indicate that approximately 85-90% of patients who accept this procedure obtain excellent hurting relief. The caste of pain relief depends largely upon the reason the procedure was done. The degree of pain relief for revision cases is a fiddling lower than for procedures done for the first time, and this is believed to be due to the scar formation and long term damage.
The reverse prosthesis also should restore some range of motion to the shoulder, only the degree of render is not as predictable as hurting relief. Nigh patients obtain the ability to reach the meridian of their heads without the need to tilt their head. Near patients run into improvement of motion in other directions, but if their rotator cuff is torn completely they may not see improvement in the ability to reach out to the side abroad from the body (called "external rotation").
The long term survival rates (that is, how long it tin can stay in the shoulder before it starts to loosen and needs to have more surgery) of the reverse prosthesis have been favorable. The opposite prosthesis has been used in France since the 1980s only was approved past the Food and Drug Assistants (FDA) in the United States in April, 2004. Equally a result, there are currently no long term studies of its use in the United states. However, the experience of shoulder surgeons and patients from Europe seem to bespeak that the prosthesis will last xv years about 90% of the time.
What are the potential complications of this procedure?
The complications of this procedure are similar to those of articulation replacements of any joint in the body. In that location are complications like to those of regular shoulder replacements and a couple unique to this prosthesis.
The almost common complication is that the humerus or arm portion (the socket) can get dislodged from the brawl (the shoulder blade function) and the prosthesis is "dislocated." Basically the 2 parts of the prosthesis are not continued anymore. This complication is more common with the contrary prosthesis than with regular shoulder replacements. Fortunately it can be managed usually by placing the arm back into the proper place and immobilizing the arm for a menstruum of time. If the prosthesis continues to dislocate then sometimes farther surgery is needed to tighten things up.
The second most common complexity of concern later on a opposite prosthesis is infection. This occurs rarely merely if it does occur it can exist frustrating for the patient and physician alike. Sometimes the infection can exist controlled by surgery to wash out the articulation and with antibiotics. If the infection becomes chronic despite handling, and so there are options for solving the infection, but they largely involve further surgery.
Another complexity of this prosthesis is that the arm portion can make contact with the bone of the shoulder blade in certain positions. This contact tin can create a groove in the bone of the shoulder blade that unremarkably is not painful. Unremarkably this complication does not require further surgery and tin exist controlled with abstention of the arm positions and with medication.
Other complications are very uncommon, just tin can rarely exist seen with this prosthesis or with regular shoulder replacements. These include tingling, numbness and weakness if the fretfulness to the arm stretched during surgery. Injury to blood vessels is very, very rare but can happen particularly when at that place is a lot of scaring and the patient has had multiple operations. Problem with medical conditions, such as blood clots in the legs (deep venous thrombosis) which can travel to the lungs (pulmonary embolus), heart attacks, strokes, drug or coldhearted reactions tin can occur with any functioning, but in our experience these are very rare afterward shoulder replacement surgery.
Who should not have a opposite prosthesis?
In that location are only a few instances where a contrary prosthesis cannot be implanted. The first is if the socket bone (of the shoulder blade or scapula) is too far gone to let the component base plate to exist able to be fixed with screws to the bone. In some instances bone graft tin can be added at the time of surgery which makes it possible to place the base plate and screws, or os graft can be added to permit placement of the base plate at a afterward appointment.
Patients with an ongoing infection in the shoulder should not have a reverse prosthesis. However, if the infection can exist cleared up so a prosthesis can be inserted. Whenever a shoulder replacement is attempted in a shoulder that has had a previous infection, the mail-operative infection rate is higher than if the shoulder never had an infection. This should be discussed in detail with your doc prior to having this surgery done.
References
-
Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The Reverse Shoulder Prosthesis for glenohumeral arthritis associated with severe rotator gage deficiency. A minimum ii-twelvemonth follow-up written report of threescore patients. J Bone Joint Surg Am 2005;87(8):1697-705
-
Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 1993;16(one):65-8.
-
Valenti P, Boutens D, Nerot Cea. Delta 3 reverse prosthesis for osteoarthritis with massive rotator cuff tear: long term results. In: Walch G, Boileau P, Mole D, editors. 2000 Shoulder Prosthesis. ii to x year follow-up. Montpellier: Sauramps Medical; 2001. p. 253-259.
-
Werner CM, Steinmann PA, Gilbart G, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III contrary-brawl-and-socket total shoulder prosthesis. J Bone Articulation Surg Am 2005;87(vii):1476-86.
-
Boulahia A, Edwards TB, Walch G, Baratta RV. Early results of a reverse design prosthesis in the handling of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics 2002;25(2):129-33.
-
Rittmeister One thousand, Kerschbaumer F. Grammont reverse full shoulder arthroplasty in patients with rheumatoid arthritis and nonreconstructible rotator cuff lesions. J Shoulder Elbow Surg 2001;10(one):17-22.
-
Sirveaux F, Favard L, Oudet D, Huquet D, Walch Thousand, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of fourscore shoulders. J Bone Articulation Surg Br 2004;86(3):388-95.
-
Hatzidakis AM, Norris TR, Boileau P. Opposite shoulder arthroplasty; Indication, Technique and Results. Techniques in shoulder and elbow surgery 2005;vi(3):135-154.
schneidermobleclat.blogspot.com
Source: https://www.hopkinsmedicine.org/orthopaedic-surgery/specialty-areas/shoulder/treatments-procedures/reverse-prosthesis.html
0 Response to "Will I Be Able to Golf Again After Reverse Shoulder Replacement"
Post a Comment